Hemoglobinuria: Unexpected Signals You Must Not Ignore
Hemoglobinuria is a rare but serious condition that may silently signal underlying health issues. While often unnoticed in early stages, certain unexpected symptoms could point to a more significant problem. Understanding these signs is essential for timely diagnosis and treatment. This article uncovers the key warning signals of hemoglobinuria and what they could mean for your health
Hemoglobinuria represents a complex medical condition where hemoglobin appears in urine due to excessive breakdown of red blood cells. This phenomenon can indicate various underlying health issues, from relatively benign causes to serious systemic disorders requiring immediate intervention.
What Are Early Signs You Might Overlook
Many individuals miss the initial warning signs of hemoglobinuria because symptoms often appear gradually or intermittently. The most obvious indicator involves changes in urine color, ranging from pink or red to dark brown or cola-colored appearance. However, early stages might present with subtle discoloration that people attribute to dehydration or dietary factors.
Fatigue and weakness frequently accompany hemoglobinuria, as the body struggles with reduced red blood cell counts. Some patients experience back pain, particularly in the kidney area, along with general malaise that worsens during episodes. Shortness of breath during normal activities can also signal the condition, especially when combined with pale skin or nail beds.
Nocturnal episodes present unique challenges, as symptoms often intensify during sleep or upon waking. Morning urine typically shows the most pronounced discoloration, making early morning observation crucial for detection.
How This Could Indicate a Deeper Health Issue
Hemoglobinuria serves as a symptom rather than a standalone disease, often pointing to more serious underlying conditions. Paroxysmal nocturnal hemoglobinuria represents one of the most concerning causes, involving a rare blood disorder where red blood cells become vulnerable to destruction by the body’s complement system.
Autoimmune disorders frequently trigger hemoglobinuria episodes, as the immune system mistakenly attacks healthy red blood cells. Conditions like systemic lupus erythematosus or autoimmune hemolytic anemia can manifest through recurring hemoglobinuria episodes alongside other systemic symptoms.
Infections, particularly those caused by certain bacteria or parasites, can lead to massive red blood cell destruction. Malaria, for example, commonly causes hemoglobinuria in affected regions, while bacterial infections like clostridial sepsis can trigger similar responses.
Genetic disorders affecting red blood cell structure or enzyme function also contribute to hemoglobinuria. G6PD deficiency, a common genetic condition, makes red blood cells susceptible to breakdown when exposed to certain medications, foods, or stressors.
Important Diagnostic Steps for Early Detection
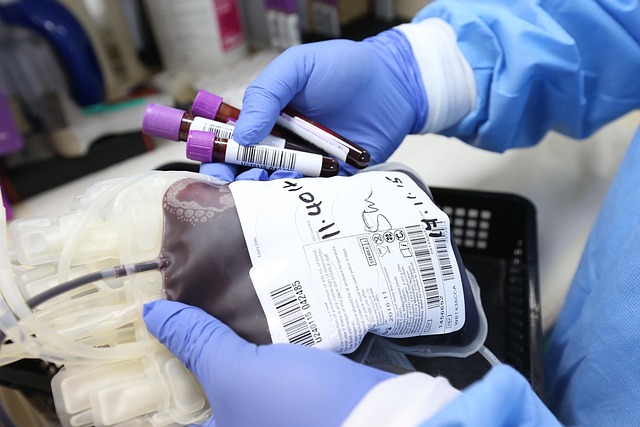
Effective diagnosis requires comprehensive evaluation combining clinical assessment with specialized laboratory testing. Initial urinalysis provides crucial information about hemoglobin presence, but additional tests help determine the underlying cause and severity.
Complete blood counts reveal red blood cell levels, hemoglobin concentrations, and signs of ongoing destruction. Peripheral blood smears allow microscopic examination of red blood cell shape and structure, identifying abnormalities that suggest specific conditions.
Specialized tests like flow cytometry can detect paroxysmal nocturnal hemoglobinuria by identifying cells lacking specific surface proteins. Coombs tests help diagnose autoimmune causes, while enzyme assays can identify genetic deficiencies like G6PD deficiency.
Kidney function tests ensure that hemoglobinuria hasn’t caused secondary kidney damage, while imaging studies might be necessary to rule out structural abnormalities or other complications.
Myths About Hemoglobin in Urine and How to Approach Them
Several misconceptions surround hemoglobinuria, potentially delaying appropriate treatment. Many people believe that red-colored urine always indicates blood in urine, but hemoglobinuria specifically involves free hemoglobin rather than intact red blood cells.
Another common myth suggests that dietary factors like beets or certain medications always cause red urine. While these can temporarily discolor urine, true hemoglobinuria involves specific biochemical processes that require medical evaluation.
Some individuals assume that intermittent symptoms don’t warrant medical attention, believing that occasional episodes will resolve spontaneously. However, even sporadic hemoglobinuria can indicate serious underlying conditions requiring ongoing monitoring and treatment.
The misconception that hemoglobinuria only affects certain age groups or demographics can also delay diagnosis. This condition can affect individuals of any age, gender, or ethnic background, depending on the underlying cause.
Treatment Options Available
Treatment approaches vary significantly based on the underlying cause and severity of hemoglobinuria. For paroxysmal nocturnal hemoglobinuria, complement inhibitors like eculizumab have revolutionized treatment outcomes, significantly reducing hemolysis episodes and improving quality of life.
Autoimmune-related hemoglobinuria often requires immunosuppressive therapy, including corticosteroids, rituximab, or other targeted medications. Treatment plans typically involve careful monitoring and gradual medication adjustments to achieve optimal results while minimizing side effects.
Supportive care plays a crucial role in managing acute episodes, including blood transfusions for severe anemia, fluid replacement to prevent kidney damage, and folic acid supplementation to support red blood cell production.
For genetic causes like G6PD deficiency, treatment focuses on avoiding triggers and managing acute episodes when they occur. Patient education about potential triggers becomes essential for preventing future episodes.
| Treatment Type | Condition | Estimated Cost Range |
|---|---|---|
| Complement Inhibitors | Paroxysmal Nocturnal Hemoglobinuria | $400,000-$500,000 annually |
| Immunosuppressive Therapy | Autoimmune Hemolysis | $2,000-$15,000 monthly |
| Blood Transfusions | Acute Episodes | $1,500-$3,000 per transfusion |
| Supportive Care | Various Causes | $500-$2,000 monthly |
Prices, rates, or cost estimates mentioned in this article are based on the latest available information but may change over time. Independent research is advised before making financial decisions.
Early recognition and appropriate treatment of hemoglobinuria can significantly improve outcomes and prevent serious complications. Working closely with healthcare providers ensures proper diagnosis and optimal treatment strategies tailored to individual needs and underlying causes.
This article is for informational purposes only and should not be considered medical advice. Please consult a qualified healthcare professional for personalized guidance and treatment.




