Hemoglobinuria: Unexpected Signals You Must Not Ignore
Hemoglobinuria, the presence of hemoglobin in urine, often serves as a warning sign for underlying health conditions that require prompt medical attention. This condition, especially in its nocturnal form, can indicate serious disorders affecting red blood cells. Understanding the early signals, proper diagnostic approaches, and available treatment options is crucial for managing this condition effectively and preventing complications.
Hemoglobinuria occurs when hemoglobin, the oxygen-carrying protein in red blood cells, appears in urine. This condition often indicates red blood cell destruction within the bloodstream, a process called intravascular hemolysis. While occasional mild cases might not cause alarm, persistent or severe hemoglobinuria requires medical attention, particularly when it manifests during sleep—a condition known as paroxysmal nocturnal hemoglobinuria (PNH). This rare acquired blood disorder affects approximately 1-1.5 people per million worldwide and can lead to serious complications if left untreated.
What Are Early Signs of Hemoglobinuria You Might Overlook?
The early manifestations of hemoglobinuria can be subtle and easily dismissed. One of the most common yet overlooked signs is dark or tea-colored urine, especially noticeable in the morning. This discoloration results from hemoglobin being excreted through the kidneys. Patients might also experience unexplained fatigue that persists despite adequate rest, which stems from the resulting anemia as red blood cells are destroyed.
Abdominal pain and discomfort, particularly around the lower back area, may indicate kidney involvement. Some individuals report mild jaundice—a yellowish tint to the skin or eyes—which occurs when bilirubin levels rise due to increased red blood cell breakdown. Headaches and difficulty concentrating can also manifest as the body struggles with reduced oxygen-carrying capacity. These symptoms may appear intermittently, making them easy to attribute to other causes or dismiss entirely.
How Hemoglobinuria Could Indicate a Deeper Health Issue
Hemoglobinuria rarely exists in isolation—it typically signals underlying medical conditions that require attention. In paroxysmal nocturnal hemoglobinuria, a genetic mutation in bone marrow stem cells leads to the production of defective blood cells vulnerable to premature destruction by the body’s complement system. This condition increases the risk of blood clots (thrombosis), which can be life-threatening if they develop in critical blood vessels.
Other conditions associated with hemoglobinuria include autoimmune hemolytic anemia, where the immune system mistakenly attacks red blood cells, and certain infections that damage blood cells. Hemoglobinuria may also result from severe physical exertion (march hemoglobinuria), exposure to certain medications or toxins, or transfusion reactions. In some cases, it can indicate serious kidney disease, as damaged kidneys may fail to properly filter hemoglobin from the bloodstream.
The appearance of hemoglobin in urine also correlates with an increased risk of pulmonary hypertension, kidney failure, and in severe cases, stroke or heart attack. Understanding these connections emphasizes why even seemingly minor episodes of hemoglobinuria warrant proper medical evaluation.
Important Diagnostic Steps for Detecting Hemoglobinuria Early
Early and accurate diagnosis of hemoglobinuria involves several key steps. Initially, healthcare providers typically order urinalysis to confirm the presence of hemoglobin in urine and distinguish it from other conditions that cause discolored urine. Blood tests, including complete blood count (CBC), reticulocyte count, and lactate dehydrogenase (LDH) levels, help assess the extent of hemolysis and resulting anemia.
For suspected paroxysmal nocturnal hemoglobinuria, flow cytometry has become the gold standard diagnostic tool. This technique detects the absence of specific proteins (CD55 and CD59) on red blood cells, which is characteristic of PNH. Bone marrow examination may be necessary to rule out other bone marrow disorders and assess the extent of the condition.
Additional tests often include the Coombs test to identify antibodies attached to red blood cells, hemosiderin staining of urine to detect past hemolysis events, and specialized tests to measure complement activity. Imaging studies such as ultrasound or CT scans may be ordered to evaluate organ involvement, particularly the kidneys and liver. Early diagnosis through these methods significantly improves treatment outcomes and helps prevent complications.
Myths About Hemoglobin in Urine and How to Approach Them
Several misconceptions surround hemoglobinuria, potentially delaying proper diagnosis and treatment. One common myth suggests that red or dark urine always indicates blood in urine (hematuria) rather than free hemoglobin. While both conditions cause similar urine discoloration, they have different causes and implications. Proper laboratory testing can distinguish between them.
Another misconception is that hemoglobinuria always causes visible symptoms. In reality, mild cases may go unnoticed, with hemoglobin detectable only through laboratory testing. Some patients mistakenly attribute their fatigue and weakness to lifestyle factors rather than recognizing them as potential symptoms of underlying hemolysis.
Many people incorrectly believe that hemoglobinuria is always caused by kidney disease. While kidney problems can result from hemoglobinuria, they are often the consequence rather than the cause. Additionally, the myth that hemoglobinuria always indicates a permanent condition prevents some individuals from seeking treatment. In fact, when caused by certain medications or infections, hemoglobinuria may resolve once the underlying trigger is addressed.
Treatment Options for Nocturnal Hemoglobinuria
Management of paroxysmal nocturnal hemoglobinuria has evolved significantly in recent years, offering improved outcomes for patients. Complement inhibitor therapy represents the most significant advancement in PNH treatment. Medications such as eculizumab (Soliris) and ravulizumab (Ultomiris) work by blocking the complement system’s attack on red blood cells, reducing hemolysis and associated symptoms.
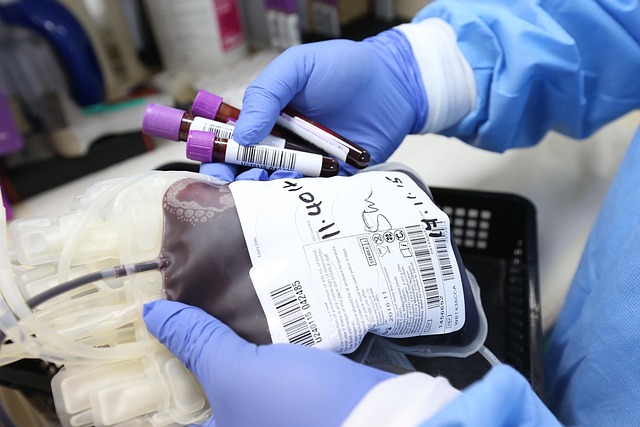
For patients with severe anemia, blood transfusions may be necessary to maintain adequate hemoglobin levels. Iron and folic acid supplementation often helps support red blood cell production, particularly in patients with ongoing hemolysis. Anticoagulant medications are frequently prescribed to reduce the risk of blood clots, a serious complication of PNH.
In selected cases, particularly for younger patients with severe disease, hematopoietic stem cell transplantation (HSCT) offers the potential for cure. This procedure replaces the patient’s bone marrow with healthy donor cells, eliminating the defective stem cells responsible for PNH. However, HSCT carries significant risks and is typically reserved for patients with severe disease who have suitable donors.
Supportive care remains essential for symptom management. This includes pain control for abdominal discomfort, management of kidney complications, and monitoring for early signs of thrombosis. Regular follow-up with hematologists experienced in treating PNH ensures appropriate adjustment of therapy as the disease evolves.
This article is for informational purposes only and should not be considered medical advice. Please consult a qualified healthcare professional for personalized guidance and treatment.




