Myelodysplastic Syndrome: Silent Signals You Shouldn’t Ignore
Myelodysplastic syndrome (MDS) represents a group of blood disorders that develop when bone marrow fails to produce healthy blood cells effectively. This condition often progresses silently, with symptoms that can easily be mistaken for normal aging or other common health issues. Understanding the warning signs and risk factors of MDS is crucial for early detection and proper medical intervention, as timely diagnosis can significantly impact treatment outcomes and quality of life.
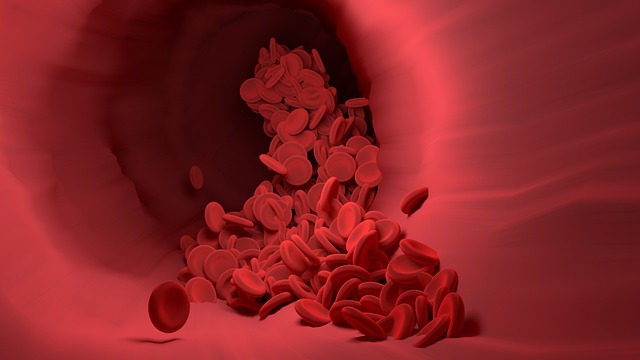
Myelodysplastic syndrome affects thousands of people annually, yet many remain unaware of its existence until symptoms become severe. This blood disorder disrupts the normal production of red blood cells, white blood cells, and platelets, leading to a cascade of health complications that can dramatically impact daily functioning.
What is Myelodysplastic Syndrome and Who is at Risk?
Myelodysplastic syndrome encompasses a collection of disorders characterized by dysfunctional bone marrow that produces abnormal blood cells. The bone marrow, typically responsible for generating healthy blood components, begins creating cells that are malformed or insufficient in number. This condition primarily affects adults over 65, with the median age of diagnosis being 70 years. Men are slightly more likely to develop MDS than women, and previous cancer treatments, particularly chemotherapy and radiation therapy, significantly increase the risk. Environmental factors such as exposure to certain chemicals, including benzene and heavy metals, also contribute to MDS development. Additionally, individuals with genetic disorders like Fanconi anemia or Down syndrome face elevated risks.
What Are the Early Warning Signs of MDS?
The early symptoms of MDS often mirror those of other conditions, making recognition challenging. Persistent fatigue represents the most common initial symptom, as reduced red blood cell production leads to anemia. Patients frequently experience shortness of breath during routine activities, weakness that doesn’t improve with rest, and pale skin or nail beds. Unusual bruising or bleeding, including frequent nosebleeds, bleeding gums, or small red spots on the skin called petechiae, indicates low platelet counts. Recurrent infections, slow-healing wounds, and fever without obvious cause suggest compromised white blood cell function. Many individuals also report dizziness, rapid heartbeat, and cold hands or feet as their body struggles to maintain adequate oxygen circulation.
Why Do These Symptoms Often Go Unnoticed?
MDS symptoms develop gradually and are frequently attributed to normal aging processes or stress-related conditions. The subtle onset means many people adapt to their declining energy levels without recognizing the underlying cause. Healthcare providers may initially treat individual symptoms rather than investigating potential blood disorders, particularly in older adults where fatigue and weakness are common complaints. The nonspecific nature of MDS symptoms leads to misdiagnosis or delayed diagnosis in approximately 40% of cases. Additionally, some individuals may have mild symptoms that don’t significantly impact their daily activities, causing them to postpone medical evaluation until the condition progresses.
How Does MDS Affect Your Body’s Blood Production?
MDS disrupts the bone marrow’s normal blood cell manufacturing process through genetic mutations that occur in stem cells. These mutations cause the production of abnormal blood cells that cannot function properly or survive as long as healthy cells. The bone marrow may appear active under microscopic examination, but the cells it produces are defective and often die before entering circulation. This results in cytopenias, or low blood cell counts, affecting one or more cell lines. Red blood cell deficiency leads to anemia and oxygen transport problems, while low white blood cell counts compromise immune system function. Reduced platelet production affects blood clotting ability, increasing bleeding risks. Over time, the accumulation of abnormal cells can transform into acute leukemia in approximately 30% of MDS cases.
When Should You Seek Medical Attention?
Immediate medical evaluation is warranted when experiencing persistent fatigue that interferes with daily activities, unexplained bruising or bleeding, or recurrent infections that don’t respond to standard treatment. Any combination of weakness, shortness of breath, and pale appearance should prompt consultation with a healthcare provider. Individuals with previous cancer treatment history should be particularly vigilant about these symptoms and maintain regular follow-up appointments. Blood tests revealing low blood cell counts during routine screenings require further investigation, even in the absence of symptoms. Early detection through complete blood count testing and bone marrow examination can confirm MDS diagnosis and enable prompt treatment initiation.
Recognizing the silent signals of myelodysplastic syndrome empowers individuals to seek appropriate medical care before complications develop. While MDS primarily affects older adults, awareness of its symptoms and risk factors enables earlier intervention and better management of this complex blood disorder. Regular medical monitoring and prompt attention to concerning symptoms remain the best strategies for addressing MDS effectively.
This article is for informational purposes only and should not be considered medical advice. Please consult a qualified healthcare professional for personalized guidance and treatment.




