Understanding Hepatitis C: Early Indicators and Key Factors That Shape Its Progression
Hepatitis C often develops quietly, with early signs that may seem mild or easy to overlook. This article explores the subtle symptoms, risk factors, and underlying influences that determine how the disease progresses and why early detection matters.
Hepatitis C represents a significant public health challenge, affecting an estimated 2.4 million people in the United States alone. This blood-borne virus targets the liver, often progressing silently over decades. Understanding the early indicators and factors that shape disease progression empowers individuals to seek timely medical evaluation and adopt protective lifestyle measures.
This article is for informational purposes only and should not be considered medical advice. Please consult a qualified healthcare professional for personalized guidance and treatment.
Early Indicators of Hepatitis C
Hepatitis C typically develops in two phases: acute and chronic. During the acute phase, which occurs within the first six months after exposure, most individuals experience no symptoms at all. When symptoms do appear, they tend to be mild and nonspecific, making them easy to dismiss or attribute to other causes.
Common early indicators include persistent fatigue that does not improve with rest, low-grade fever, muscle aches, joint pain, and mild abdominal discomfort concentrated in the upper right quadrant where the liver is located. Some people notice a loss of appetite, nausea, or unexplained weight loss. In rare cases, jaundice may develop, characterized by yellowing of the skin and eyes, dark urine, and pale-colored stools. These symptoms result from the liver’s reduced ability to process bilirubin, a waste product from red blood cell breakdown.
Because these signs are often subtle or absent entirely, many people only discover their infection through routine blood work or when donating blood. The Centers for Disease Control and Prevention recommends that all adults aged 18 and older receive at least one hepatitis C screening test in their lifetime, with more frequent testing for those at higher risk.
Why Hepatitis C Often Remains Undetected
The silent nature of hepatitis C contributes significantly to delayed diagnosis. Unlike hepatitis A or B, which often cause noticeable acute illness, hepatitis C typically establishes chronic infection without triggering obvious symptoms. The liver itself has no pain receptors, meaning significant damage can accumulate before any physical discomfort alerts the individual to a problem.
Approximately 75 to 85 percent of people with acute hepatitis C develop chronic infection, yet many remain asymptomatic for 20 to 30 years. During this time, the virus steadily damages liver tissue, potentially leading to fibrosis, cirrhosis, or hepatocellular carcinoma. The gradual progression allows the body to compensate for declining liver function until damage becomes extensive.
Historical factors also contribute to undetected cases. Before 1992, when blood supply screening became standard practice, many individuals contracted hepatitis C through transfusions or organ transplants. Others were exposed through injection drug use, unsterile medical procedures, or occupational needle-stick injuries. The stigma associated with certain transmission routes may discourage some individuals from seeking testing, further delaying diagnosis.
Additionally, healthcare providers may not always screen for hepatitis C unless specific risk factors are present or liver enzyme abnormalities appear on routine blood tests. This reactive rather than proactive approach means infections can persist unrecognized for extended periods.
How Lifestyle Factors Influence Liver Function
Once hepatitis C infection is established, various lifestyle factors can accelerate or slow disease progression. The liver performs over 500 essential functions, including filtering toxins, producing proteins, and regulating metabolism. Supporting liver health through conscious lifestyle choices becomes particularly important for those living with chronic viral hepatitis.
Alcohol consumption represents one of the most significant modifiable risk factors. Even moderate alcohol intake can accelerate liver damage in people with hepatitis C, increasing the risk of cirrhosis and liver cancer. Healthcare professionals typically recommend complete alcohol abstinence for individuals with chronic hepatitis C.
Obesity and metabolic syndrome also negatively impact liver health. Excess body weight, particularly visceral fat accumulation, promotes fatty liver disease, which compounds the inflammation and scarring caused by hepatitis C. Maintaining a healthy weight through balanced nutrition and regular physical activity helps protect liver function and may slow fibrosis progression.
Dietary choices matter as well. A diet rich in fruits, vegetables, whole grains, and lean proteins provides essential nutrients that support liver repair and regeneration. Conversely, excessive consumption of processed foods, saturated fats, and added sugars can burden the liver and contribute to metabolic dysfunction.
Certain medications and supplements require careful consideration, as the liver metabolizes most substances entering the body. Some over-the-counter pain relievers, particularly acetaminophen in high doses, can cause additional liver stress. Individuals with hepatitis C should always consult healthcare providers before starting new medications or supplements.
Smoking tobacco has been associated with faster progression of liver fibrosis and increased risk of liver cancer in people with chronic hepatitis C. Smoking cessation represents another important protective measure.
Understanding How the Body Reacts to Viral Liver Stress
The hepatitis C virus triggers a complex immune response that paradoxically contributes to both viral clearance attempts and liver damage. When the virus enters liver cells (hepatocytes), it hijacks cellular machinery to replicate. The immune system detects this intrusion and mounts a response involving various immune cells and inflammatory molecules.
In acute infection, a robust immune response may successfully eliminate the virus in about 15 to 25 percent of cases. However, hepatitis C has evolved mechanisms to evade immune surveillance, allowing it to establish persistent infection in most individuals. The virus exhibits high genetic variability, rapidly mutating to escape antibody recognition and T-cell attacks.
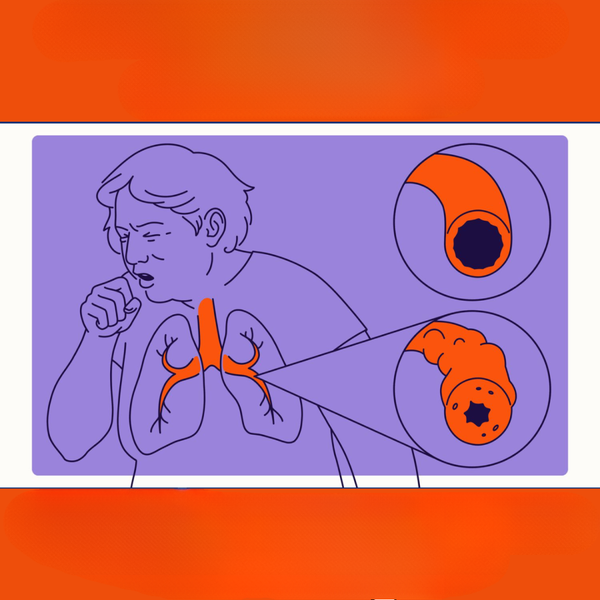
Chronic inflammation becomes the hallmark of persistent hepatitis C infection. Immune cells continuously infiltrate liver tissue, releasing inflammatory cytokines and enzymes that damage hepatocytes. While this response aims to eliminate infected cells, it inadvertently harms healthy tissue as well. Over time, repeated cycles of cell death and regeneration lead to fibrosis, the accumulation of scar tissue that gradually replaces functional liver tissue.
The liver possesses remarkable regenerative capacity, but chronic viral stress eventually overwhelms this ability. As fibrosis progresses to cirrhosis, the liver’s architecture becomes distorted, blood flow is impeded, and synthetic functions decline. Portal hypertension may develop, leading to complications such as varices, ascites, and hepatic encephalopathy.
Interestingly, the severity of immune response varies among individuals, influenced by genetic factors, age at infection, sex, and coexisting conditions. Some people experience rapid disease progression, while others maintain stable liver function for decades despite chronic infection. This variability underscores the importance of regular medical monitoring and individualized treatment approaches.
Advances in antiviral therapy have revolutionized hepatitis C management. Direct-acting antiviral medications can now cure over 95 percent of infections, typically within 8 to 12 weeks of treatment. These medications work by targeting specific viral proteins essential for replication, effectively stopping the infection and allowing the liver to begin healing. Early treatment, before significant fibrosis develops, offers the best outcomes and can prevent progression to cirrhosis and liver cancer.
Conclusion
Hepatitis C remains a significant health concern, but increased awareness of early indicators and progression factors enables better outcomes. The often-silent nature of this infection emphasizes the importance of routine screening, particularly for at-risk populations. Recognizing subtle symptoms, understanding why detection is frequently delayed, adopting liver-protective lifestyle habits, and appreciating how the body responds to viral stress all contribute to more effective disease management. With modern antiviral treatments offering high cure rates, early diagnosis and intervention can prevent serious complications and restore liver health. Anyone concerned about hepatitis C exposure should consult a healthcare provider for appropriate testing and guidance.




