Understanding HIV: Early Indicators and Key Factors in Its Progression
HIV can develop quietly, with early signs that are often subtle and easy to overlook. Many people may not notice symptoms at first or may mistake them for common illnesses, which can delay diagnosis and treatment. This article explores the early indicators to watch for, explains how symptoms can change over time, and highlights the key factors that influence how the condition progresses. Understanding these signs and seeking timely testing can play a crucial role in managing HIV effectively and maintaining long-term health.
Human Immunodeficiency Virus continues to affect populations across the United States and globally, making awareness and education critical components of public health. While medical advances have transformed this condition into a manageable chronic illness, early detection remains vital for optimal outcomes. Understanding the initial signs, the reasons they often remain unrecognized, and the factors that influence how the body responds to viral challenges can empower individuals to seek appropriate medical care promptly.
This article is for informational purposes only and should not be considered medical advice. Please consult a qualified healthcare professional for personalized guidance and treatment.
What Are Early Indicators of HIV?
The initial phase of infection, known as acute retroviral syndrome, typically occurs within two to four weeks after exposure. During this period, the virus multiplies rapidly, and the immune system begins mounting a response. Common early indicators include fever, fatigue, swollen lymph nodes, sore throat, rash, muscle aches, and headaches. These symptoms resemble those of common viral infections like the flu or mononucleosis, which contributes to their frequent misidentification. Not everyone experiences noticeable symptoms during this stage, and the severity can vary significantly among individuals. Some people may have mild symptoms that resolve quickly, while others experience more pronounced effects lasting several weeks. The presence of these indicators does not confirm infection, but their occurrence following potential exposure warrants immediate medical evaluation and testing.
Why HIV Symptoms Often Go Unnoticed
Several factors contribute to the frequent oversight of initial infection signs. The nonspecific nature of early symptoms makes them easily attributable to common illnesses, leading many individuals to dismiss them without seeking medical attention. The acute phase symptoms typically resolve on their own within a few weeks, after which the virus enters a chronic asymptomatic phase that can last for years. During this latent period, individuals may feel completely healthy despite ongoing viral replication and gradual immune system damage. Additionally, many people lack awareness of their potential exposure risk or do not associate their symptoms with the possibility of infection. Stigma and fear surrounding testing can also prevent individuals from seeking timely medical evaluation. The absence of routine screening in many healthcare settings means infections may remain undetected until more advanced stages, when immune function has significantly declined. This delay in diagnosis reduces the effectiveness of treatment and increases the risk of transmission to others.
How Lifestyle and Health Factors Affect Immune Function
The immune system’s ability to respond to viral challenges depends on numerous interconnected factors. Nutritional status plays a fundamental role, as deficiencies in essential vitamins and minerals can impair immune cell production and function. Adequate protein intake supports antibody production, while micronutrients like vitamin D, zinc, and selenium contribute to various immune processes. Chronic stress elevates cortisol levels, which can suppress immune responses and increase susceptibility to infections. Sleep quality and duration directly impact immune function, with insufficient rest reducing the production of protective cytokines and infection-fighting antibodies. Physical activity influences immune health in complex ways; moderate exercise generally enhances immune surveillance, while excessive training without adequate recovery can temporarily suppress immune function. Substance use, particularly alcohol and tobacco, compromises immune defenses through multiple mechanisms, including impaired barrier function, altered immune cell activity, and increased inflammation. Pre-existing health conditions such as diabetes, cardiovascular disease, and chronic kidney disease can further compromise immune responses and complicate disease management.
Understanding How the Body Responds to Viral Stress
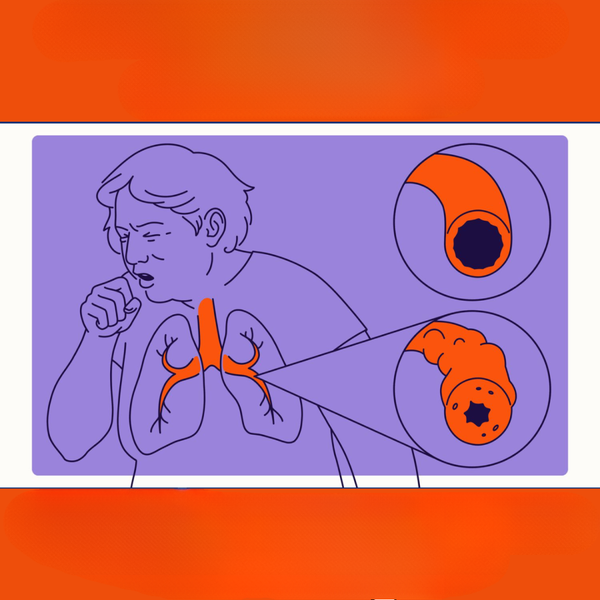
When a virus enters the body, the immune system initiates a coordinated response involving multiple cell types and signaling molecules. The innate immune system provides immediate, nonspecific defense through physical barriers, inflammatory responses, and natural killer cells. Meanwhile, the adaptive immune system develops targeted responses through T cells and B cells, which recognize specific viral proteins and generate immunological memory. In the case of this particular virus, the pathogen specifically targets CD4+ T cells, which are crucial coordinators of immune responses. As these cells become infected and destroyed, the immune system gradually loses its ability to mount effective defenses against various pathogens. The body attempts to compensate by producing more CD4+ cells, but viral replication eventually outpaces this production in untreated individuals. Chronic immune activation resulting from persistent viral presence leads to inflammation and immune exhaustion, where immune cells become less responsive over time. This process explains why untreated infection eventually progresses to acquired immunodeficiency syndrome, characterized by severe immune compromise and vulnerability to opportunistic infections. Modern antiretroviral therapy interrupts viral replication, allowing immune function to stabilize or partially recover, demonstrating the importance of early treatment initiation.
Understanding the progression of infection requires recognizing that each individual’s experience differs based on genetic factors, viral characteristics, and overall health status. Some people naturally control viral replication better than others due to specific genetic variations affecting immune responses or viral entry mechanisms. The viral strain itself can influence disease progression, with some variants replicating more aggressively than others. Co-infections with other pathogens can accelerate immune decline and complicate clinical management. These variables underscore the importance of personalized medical care and regular monitoring for anyone diagnosed with the condition.
Advances in medical treatment have dramatically improved outcomes for people living with this condition. Early diagnosis followed by consistent antiretroviral therapy can reduce viral loads to undetectable levels, preserve immune function, and prevent transmission to others. Regular medical monitoring allows healthcare providers to adjust treatment as needed and address any complications promptly. Preventive measures, including pre-exposure prophylaxis for high-risk individuals and post-exposure prophylaxis following potential exposure, have added important tools for reducing new infections. Public health efforts focusing on education, stigma reduction, and accessible testing continue to play vital roles in controlling the epidemic.
Recognizing early indicators, understanding why symptoms may be overlooked, and appreciating the complex factors affecting immune function and viral response are essential steps toward better health outcomes. Anyone concerned about potential exposure should seek confidential testing and medical consultation regardless of symptom presence. Early intervention remains the most effective strategy for managing this condition and maintaining quality of life.




